Hyperpigmentation Condition
Hyperpigmentation Condition
Pigmentation is a complex condition that concerns many clients. In fact, in my clinical work, the complaints about pigmentation from clients exceed that of aging.
Why are treatments for this condition failing? It is a multi-faceted question, and the reasons can be numerous, so, let's review the pigmentation process called melanogenesis to explore some answers.
The melanocyte is the name of the cell responsible for the formation of pigment that colours our skin, hair, and eyes. It is formed during the embryonic stage in the neural crest. As the fetus develops the melanocytes migrate away from the neural crest, travelling through the body to the areas where pigment is usually found (the skin hair and eyes). Over 120 genes are involved in this cell movement and hence the potential for 120 reasons where something could go wrong.
Melanocytes are genetically programmed before it leaves the neural crest with a blueprint that predetermines the colour of our skin, hair, and eyes.
Research highlights some reasons why the skin condition pigmentation is so challenging to treat:
- There is no stem cell resource for melanocytes. Once the melanocyte has left the neural crest there is no return and no further development of this cell after birth.
- By the age of eighteen, the few regeneration cycles of the melanocyte have been completed.
- From the age of thirty-five, we lose 10%-20% of functioning melanocytes every ten years.
- Melanocytes will eventually settle in the lowest region of the epidermis (basal layer), just above the dermal-epidermal junction that separates the epidermis from the dermis.
- Here, about one in every ten cells is a melanocyte
- With a ratio of 1 melanocyte to 30 keratinocytes (the leading cell of the epidermis)
The melanocyte is a dendritic cell that is long-lived and has slow cycling. This long-life cycle makes them highly susceptible to Oxidative Stress, leading to Lipid Peroxidation and ultimately mitochondria DNA damage due to its long but slow-cycling life cycle.
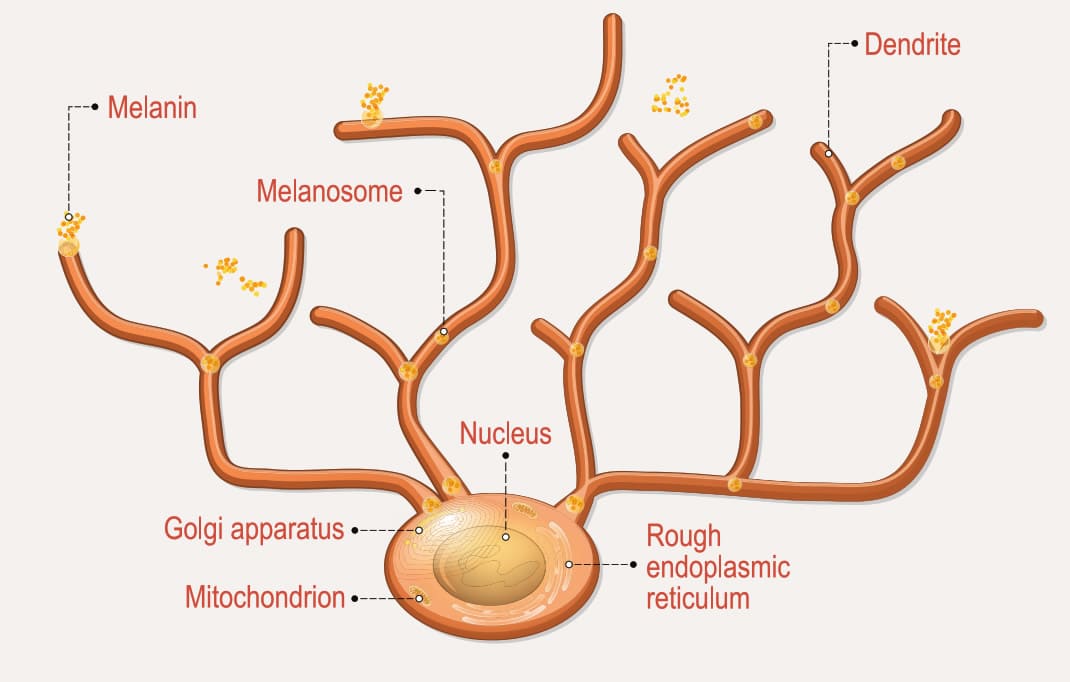
The melanocyte produces and distributes the pigment melanin which is responsible for the colour of our skin with two pigments: eumelanin, the dark brown pigment, and Pheomelanin, the red pigment. Melanin is an extremely complex polymer, and there may be very minute differences between the melanin of different people and within races.
Our skin has a different colour in different areas. This is because there are more melanocytes in darker areas such as the neck, versus lighter areas like the face. However, within these areas, the concentration of about 1000 to 2000 melanocytes per cubic millimetre is the same for all race groups.
So, whether you are a black-skinned person or a pale-skinned person, you will still have about the same number of melanocytes, BUT a different balance of eumelanin and pheomelanin pigment granules inherited from the family gene pool.
There are some significant differences between black and white skins; the most significant is that the melanocyte dendrite in black skins is longer in length.
This length enables the melanocyte to deposit pigment higher in the upper spinosum layer, affording earlier and greater protection from the hot, sunny climates in the countries from which many black skins originate.
The opposite is found in lighter skin, and here the shorter dendrites place the pigment more horizontally through the spinosum layer. The melanosomes themselves, and pigment granules are also smaller in lighter skin.
The melanocyte stands fourth-in-line of skin barrier defence, preceded by:
- Antimicrobial Barrier (previously referred to as the acid mantle)
- Permeability Layer (previously referred to as the corneocytes and multilamellar structure)
- Langerhan Cell
- Melanocyte
Individuals with a gene called melanocortin-1 receptor (red hair in the family gene pool) may have a high percentage of the red pigment pheomelanin, and this is reflected by a very short burn time. Redheads are known to have a greater risk of melanoma. The Melanocortin-1 receptor gene determines your tanning potential, but make no mistake, and it does not mean that those with fair skin cannot tan. The skin will attempt to protect itself, but tan, in this case, comes with the risk of pigmentation, loss of pigmentation and permanent damage to the melanocyte.
The formation of melanosomes and melanin pigment is a process that requires much energy from the melanocyte mitochondria creating many radicals.
This oxidative process is controlled by our built-in cellular defence antioxidant super dismutase oxide, sometimes known as superoxide dismutase. Sadly, this built-in defence system declines with cellular age or may be lost due to mitochondria DNA damage, or cellular senescence. The creation of the red pigment pheomelanin causes even more oxidative stress than the formation of the brown pigment eumelanin.
Thus, it is important to note: Repeated unprotected sun exposure or sunburn may cause the pheomelanin to become altered in such a way as to allow it to become converted into a free radical, generating the superoxide anion, which can damage nearby skin cells, including the mitochondria DNA of melanocytes, and keratinocyte stem cells. (We call this Intra-cellular oxidative stress).
Now that we have reviewed these points about the melanocyte cell, next we must understand the steps involved in the formation of the melanin pigment. It is a complex process I will try to keep simple and relevant.
We have covered some of the essential points about the melanocyte cell, and we will now go through the steps of the formation of the melanin pigment. Let us simplify what is a complex process to make it easy to understand and follow.
Essential points about the melanocyte cell
 STEP ONE:
STEP ONE:
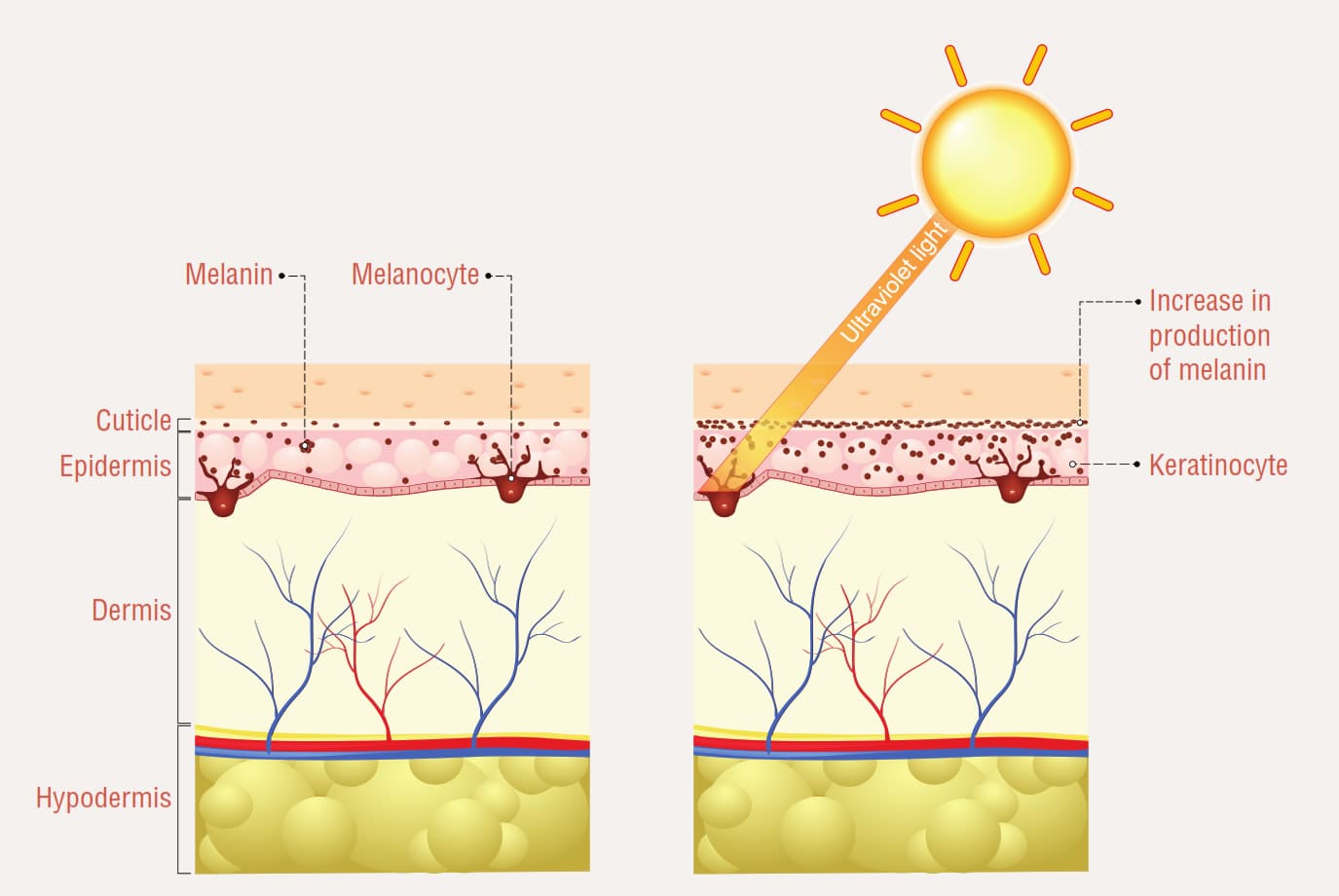
- Exposure to UltraViolet Radiation via the retina of the eye begins the melanin production process.
- UVR stimulates the pituitary gland to form a protein called Proopiomelanocortin (the precursor to the Melanin Stimulating Hormone).
- MSH first adheres to the specific receptor protein within the cell membrane of the keratinocyte.
- The keratinocyte will then communicate with the melanocyte to turn on an MSH receptor. When a molecule of MSH binds to a receptor, a series of events occur; in this instance, it will be the first step in the formation of the melanosome that will eventually carry the pigment granules eumelanin and pheomelanin.
STEP TWO:
- The enzyme tyrosinase plays a key role in melanin synthesis as a catalyst for the amino acid tyrosine, and the formation of a pre-melanosome within the melanocyte.
- Within the melanosome, pigment granules of melanin are synthesized.
- Tyrosine converts to dopa-quinone, and then to eumelanin the brown pigment, and combining dopa-quinone with cysteine, makes pheomelanin the red pigment. It is during • formation of the red pigment pheomelanin that large amounts of energy are used, and radicals created aggravating oxidative stress within the melanocyte cell.
- Melanin pigment granules are formed within the melanosome. Melanosomes are small oval pods with thread-like structures within them.
- The melanin pigment granule is deposited on these threads in varying concentrations depending on the individual genetic code. (For example, five brown and eight red pigment granules.)The melanin pigment granules inside the melanosome at this time remain almost colourless until after the transfer to the keratinocyte.
STEP THREE:
- The melanosomes pass down through the dendrites, maturing as they move.
- Once they reach the end of the dendrite, they will be transferred to the keratinocyte via a receptor called PAR-2 by phagocytosis, where they are dispersed into the cytoplasm, eventually settling over the nucleus.
- Here plays an essential role in cell defence by protecting the Nucleus DNA of the cell.
In Caucasian skin, this process occurs mostly around the lower spinosum layer. - Once the melanosome has been transferred into the cytoplasm of the keratinocyte, it becomes darker, and more visible as skin colour. This is called immediate pigment darkening.
STEP FOUR (the aftermath):
- The keratinocyte cell will then continue its journey upward to the stratum corneum
- All things going well the keratinocyte will desquamate.
The use of tanning beds or high levels of sun exposure will speed up melanogenesis. This results in increased melanosome transfer to the keratinocyte and an increase in turnover of the keratinocytes to pick up the melanosomes.
Keep in mind the increased oxidative stress from the heat, and light spectrum of UVR, including increased mitochondria energy, and resulting in oxidative stress that may result in reduced cellular energy, and production.
 So, we come back to ask the question. If all pigment gets passed to the keratinocyte and all keratinocytes desquamate; why does the skin condition pigmentation exist?
So, we come back to ask the question. If all pigment gets passed to the keratinocyte and all keratinocytes desquamate; why does the skin condition pigmentation exist?
We must understand that there are more cells and systems involved in the colour story of our skin. Aside from the melanocyte (the cell of the main discussion here), note that the keratinocyte, the innate immune system, circulatory system, and adaptive immune system all contribute to colour.
The main reason we are not getting the best results for our clients struggling with pigmentation merely is that we do not take the time to think through the process well enough to determine the best home care and in-clinic treatment program for the individual in front of us.
If the skin barrier is not functioning well to start with, then the results obtained will be limited at best. Skin health is equally as important as choosing the treatment modality. It is also vital to provide treatments in the right season to prevent an even higher risk of pigmentation for our clients.The answers, of course, lie in an in-depth consultation process.
Ask yourself many questions too. Here are some of the questions I think about when a client presents with pigmentation:
Why would there be an abnormal increase in pigment carrying melanosomes?
Pregnancy or medications such as oral contraceptive, in-vitro fertilization medication or progesterone-based medication. These cause the pituitary gland to make too much melanin-stimulating hormone.
When this happens, the MSH is continuously adhering to the receptors of the keratinocyte, and in turn, the melanocyte creates uncontrolled manufacturing of melanosomes.
This uncontrolled release of the melanin-stimulating hormone is called the MSH cascade and will be reflected in the butterfly pattern of pigmentation that is commonly seen in the center of the face.
Across the upper lip and forehead. Here is a before and after image of good results with no clinical treatments as an intervention. It was accomplished over 18 months with appropriate skin care only. (I simply illustrate the importance of improving cellular health)
What would stop the keratinocyte from picking up melanosomes?
The keratinocyte cell membrane is not viable or flexible enough to practice the phagocytosis method of picking up the melanosomes that have been transferred to the keratinocyte via a receptor called PAR-2. Essential Fatty Acid Deficiency is often the leading cause here, and if the keratinocyte is not viable or flexible the melanocyte may also be in a compromised state.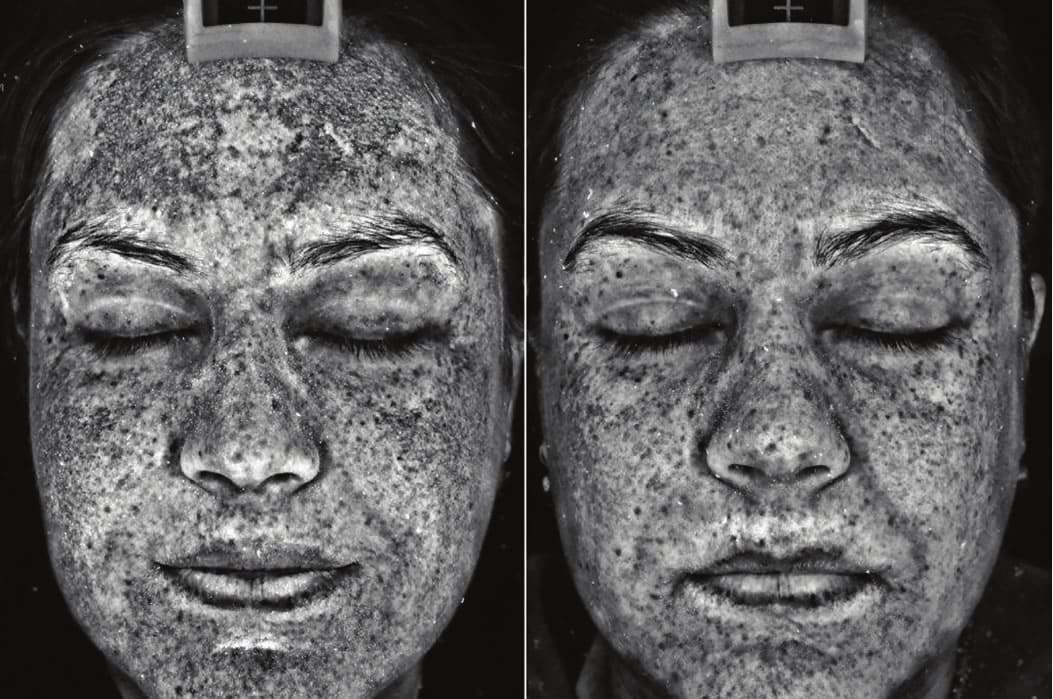
Where will the melanosome fall if not picked up by a keratinocyte?
Our knowledge about the skin’s structure tells us that the keratinocyte mother cell and melanocytes are attached to the basal lamina of the dermal-epidermal junction by keratin filaments called hemidesmosomes. This junction is permeable and also referred to as the dermo junction. The dermo junction is made of sinusoidal connective tissue, because it is filled with holes, pockets, and channels that allow the movement of fluids, and immune cells (like the Langerhans) to move through from the dermis to the epidermis. The epidermal side of this junction is called the basal lamina and is where the melanosome would rest if not picked up by the ascending keratinocyte. If this is ongoing, then a large amount of pigment could accumulate into this junction.
All of the accumulated pigment that was in the junction will be released into the dermis as a result if (or should we say, when) the dermal-epidermal junction collapse. This is called dermal pigmentation.
What will be the result if the spinosum layer were not viable enough for the even dispersion of pigment?
There will be an accumulation of pigment into smaller areas, which may reflect as pigmentation.
What will be the result if the melanocyte to keratinocyte ratio were not the normal 1-30?
The melanocyte is programmed to make a specific number of melanosomes relative to the strength and length of sun exposure it has experienced. These melanosomes should be released across thirty keratinocytes for pickup. If the melanocyte dendrites are not long enough to reach thirty keratinocytes, or there is a lesser number of keratinocytes to pick up the melanosomes, it is likely that the thirty cells are worth of melanosomes will be released out to fewer keratinocytes. It would reflect in a heavy deposition of pigment into a very small area, with many melanosomes spilling into the dermal-epidermal junction.
Today we live in a world of mixed ethnicities, and in countries other than our origin. There are many hidden dangers, and hair and eye colour as an indication to establish phototype are now misleading. The melanocortin-1 receptor gene (redhead gene) can be hidden as a result of mixed ethnicity, and this means that the client's risk for skin cancer may not be obvious.
The answers lie in the consultation, and sensible questions should cover information gathering about genetic heritage, tanning ability, redhead gene, and sunbed usage.
We have powerful treatment modalities available to us today, but they are not without risk, and just because we have a modality available does not make it the right choice for all clients with pigmentations. It is our professional obligation to say no when a client carries too high a risk. We should recommend treatment at a future date if the client is seeking treatment in a high-risk time such as summer and we can minimize risk by delaying treatment. We must say no when a client might be non-compliant with the necessary home care protocols to perform safe and effective treatments.
Above all, it is our privilege to educate our clients and give them every opportunity to fully informed consent.
References:
1. http://www.pastiche-training.com/flosaid/understanding-dermal-pigmentation
WEBPAGE TITLE: Understanding Dermal Pigmentation - Pastiche Training
2. https://www.pastiche-training.com/flosaid/understanding-dermal-pigmentation WEBPAGE TITLE: Understanding Dermal Pigmentation - Pastiche Training
3. https://emaniocreativecom.ipage.com/files/product-information/white-papers/skin- conditions/THE-MELANOCYTE-AND-COLOUR-OF-SKIN.pdf
WEBPAGE TITLE: The Melanocyte and Colour of Skin - iPage
4. https://www.pastiche-training.com/a-z-pigmentation
5. http://www.beautymagonline.com/beauty-articles-2/934-photo-allergy-2W
WEBPAGE TITLE: Photosensitivity - Beauty Mag Online
6. http://www.beautymagonline.com/beauty-articles/1199-the-power-of-the-consultation WEBPAGE TITLE: Power of The Consultation - beautymagonline.com
7. https://ghr.nlm.nih.gov/gene/MC1R
WEBPAGE TITLE: Mc1r Gene - Genetics Home Reference
8. https://www.hindawi.com/journals/ijcb/2014/709828/
WEBPAGE TITLE: Formation And Regulation Of Mitochondrial Membranes
9. https://introducingorganelles.weebly.com/mitochondria-and-golgi-apparatus.html WEBPAGE TITLE: Mitochondria And Golgi Apparatus - Organelles
10. https://articles.mercola.com/sites/articles/archive/2011/05/16/all-about-antioxi WEBPAGE TITLE: All About Antioxidants: An Important Dietary Component
11. https://ghr.nlm.nih.gov/primer/basics/mtdna
WEBPAGE TITLE: What Is Mitochondrial Dna? - Genetics Home Reference
12. Agarwal RS, Sohal RS. 1996. Relationship between susceptibility to protein oxidation, aging, and maximum life span potential of different species. Exp Gerontol, 31:365–72.
13. Jean L Bolognia & Seth J Orlow, “Melanocyte Biology” Pigmentary Disorders. Page 44.
14. Guiseppe Prota, PhD University of Naples, “Melanins & Melanogenisis; Recent applications & Perspectives” Advanced Technology conference Proceedings.
15. Dr Des Fernandes, Plastic Surgeon, “The Melanocyte & the Colour of Skin” Cape Town, South Africa.
16. Fitz chart
17. “Red-hair gene tied to melanoma” 19th Oct 2000, www.keratin.com 26th March 2004 [27] John M Pawelek et al., ”Ultraviolet light and pigmentation of the skin” Cosmetic & Toiletries, Vol 107, Nov 1992.
18. “Note for Guidance on Photo-safety Testing”, The European Agency for the Evaluation of Medicinal Products, London, 27th June 2002
19. “Some substances which cause photosensitivity”, National Occupational health & Safety Commission, www.geocities.com/fragranceallergy
20. Andrew D Montemarano, DO, “Melasma”, eMedicine, www.emedicine.com/DERM/topic260.htm 31st March 2004
21. Jason F Okulicz, MD, et al., “Lentigo” eMedicine, www.emedicine.com/DERM/topic221htm 31st March 2004
22. Shane G Silver, MD, “Ephelides”, eMedicine, www.emedicine.com/topic121.htm 31st March 2004
23. Lana H Hawayek, MD, “Poikiloderma of Civatte” , eMedicine, www.emedicine.com/derm/topic603.htm 31st March 2004
24. Ai-Lean Chew MBChB, et al., “Berloque Dermatitis”, eMedicine, www.emedicine.com/derm/topic52.htm 31st March 2004
25. Nadia I Kihiczak, MD, et al., “Postinflammatory Hyperpigmentation”, eMedicine, www.emedicine.com/derm/topic876.htm 31st March 2004
This article was first published in DERMASCOPE Magazine, April 2019, page 31, Volume 44, Issue 4