Our skin is colonized by microorganisms, bacteria, fungi and viruses, sometimes even mites. All together, they form the so-called skin microbiome and are essential for our health. At the same time, the composition of our microbiome is as individual as a fingerprint. And it affects not only our skin health but overall our well-being and possibly also our behaviour.
Our skin is colonized by microorganisms, bacteria, fungi and viruses, sometimes even mites. All together, they form the so-called skin microbiome and are essential for our health. At the same time, the composition of our microbiome is as individual as a fingerprint. And it affects not only our skin health but overall our well-being and possibly also our behaviour.
Genomic research successfully completed
In 2003, the National Institute of Health (NIH) declared that research on the human genome project was successfully completed after 13 years. We recall that we wanted to sequence the entire human genome in order to recognize hereditary diseases and to attribute other human traits (such as race) to their DNA. However, we humans are very similar in our genetic makeup. The small changes in the DNA are not responsible for the huge variations of the phenotype [1-4]. All this led to the investigation of a much larger biome - the human microbiome.
 The human microbiome project (HMP)
The human microbiome project (HMP)
The trigger for this Herculean task is the insanely important role that microbes play in our daily lives. At the same time, we humans were very reckless in dealing with antibiotics and now find multi-resistant pathogenic germs in several places. These cannot be controlled by conventional means:
- Industrial livestock farming [5]
- Hospital germs
- Epidemic spread of multidrug-resistant tuberculosis bacteria e.g. in Eastern Europe, India, South East Asia and sub-Sahara Africa [6, 7]
The publications of the human microbiome project are all listed by the NIH under the web address: https://hmpdacc.org/. The NIH is putting it like this:
“Within the human body, it is estimated that there are 10x as many microbial cells as human cells. Our microbial partners carry out a number of metabolic reactions that are not encoded in the human genome and are necessary for human health. Therefore when we talk about the "human genome" we should think of it as an amalgam of human genes and those of our microbes.”
The research on the human microbiome
The research on the HMP is not just about gaining insight, but a much bigger dimension: how to identify how microbes affect our health. That they do so has been suspected for some time. Now, also the scientific data accumulate, supporting that idea.
The relevance of this research is reflected in key parameters:
Intensive cooperation of the research groups- Creation of large research collectives
- Constant up-date of taxonomic databases [8])
- Constant improvement of analytical methods [(9]
And probably the most important:
- Publication of the vast majority of articles as "open access", i.e. they are thus freely accessible to the general public.
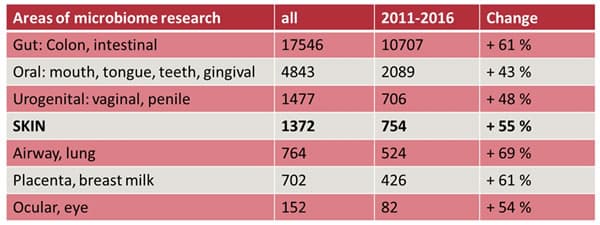
Table 1: Different areas of microbiome research [10]. It should be noticed, that most studies have been undertaken on the microbiome of the gut. However, overall intensified research of the microbiome as a whole has taken place in recent years. So also data accumulate that we humans are probably colonized with microbes everywhere.
The skin microbiome
Our skin – compared to the rest of our body and the internal organs - is an extremely dry area. . This lies in the nature of the matter because the skin forms the largest and most external human organ with a size of about 1.8 m2. At the same time, it forms an effective barrier [11, 12] against all external influences [13]. It is both flexible and supple, but also tough and resistant at the same time.
The skin surface can be grouped three main areas: oily, moist and dry (Figure 2). Actually, they are not related to the cosmetic classification of skin types[14].

Figure 2: Sketch of the different skin areas. General colour coding is used. Blue = oily, green = moist, pink = dry. Oily skin areas are located in the upper third of the body, they are also areas that are often hairy, e.g. head. Moist areas are found where there are folds of skin, e.g. in the armpit or, where many sweat glands are located as on the palms and soles of the feet. The other areas are regarded as dry, especially the extremities.
It is now logical that these areas also should have different microbial properties. That means these areas should be colonized by different members of the microbiome. The group of Elizabeth Grice [15] has been researching the skin microbiome for more than 10 years. Bacteria are the most common colonizers of the skin, followed by viruses and fungi (Figure 3). The following bacterial phylae (strains) are most commonly found: Actinobacteria, Bacteroides, cyanobacteria, firmicutes and proteobacteria.
However, one has to be careful when using the numbers from publications, because all previously found values for populations should not be considered absolute. The sampling and analysis method significantly affect the results [9]. Nevertheless, they give a good estimate.
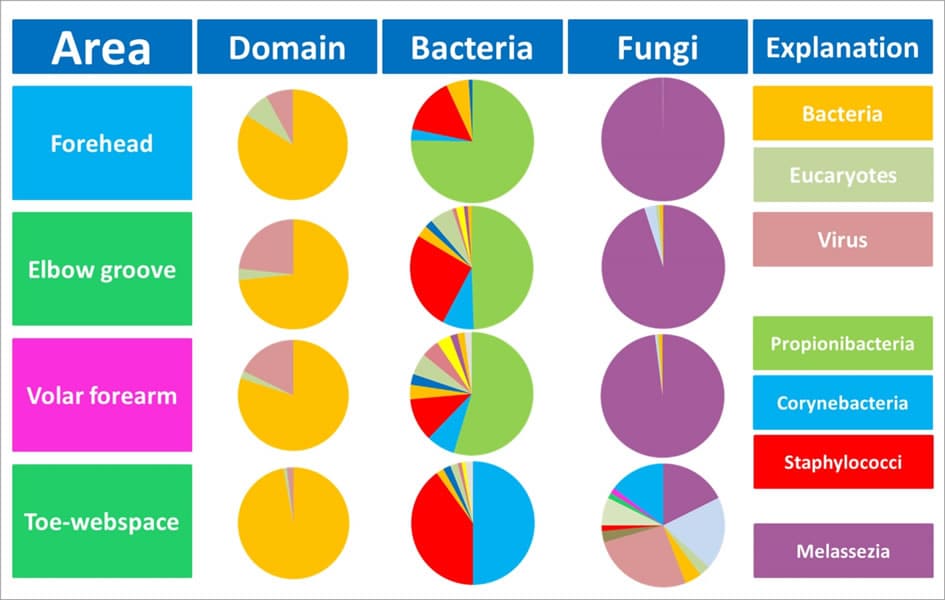
Figure 3: The different skin areas and their colonization with microbes. Bacteria - corynebacteria, staphylococci and propionibacteria - are the most frequently found bacterial members on almost every area of the skin. In addition to viruses, the fungus Malassezia is an important representative of the microbiome of the skin [16]. The diversity of the fungi is greatest on the feet, but with very low population density [17].
Recent hypotheses assume that we have inherited our very specific microbiome from our mothers (18), as well as amount and composition [19-21] which varies dramatically depending on the individual, but also in an individual himself. A solid statement, like what a healthy microbiome has to look like, cannot be done that way. However, the most important factor influencing both our microbiome of the skin and the microbiome of the gut is urbanization and the accompanying changes in our lifestyle [18].
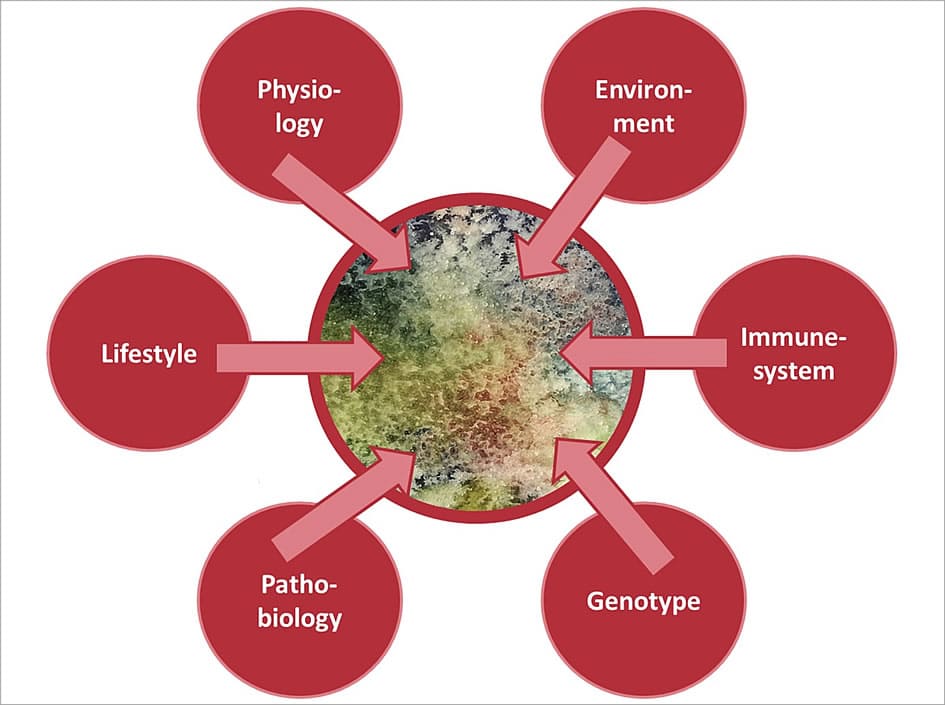
Figure 4. Important factors influencing the composition of the microbiome include physiology (age and gender), environment (climate and geographical location), immune system, genotype, lifestyle and pathobiology (e.g., diabetes) [22]. Urbanization and the concomitant changes in our lifestyles are currently regarded as the most important factors influencing our microbiome [18].
Healthy skin and the bacteria associated with
The skin surface is predominantly colonized by bacteria, to a lesser extent also by fungi and viruses. However, the latter is difficult to study in comparison to bacteria. And so research has focused mostly on the bacterial composition of the skin microbiome. Bacteria are evolutionary the oldest organisms and belong to our innate immune system. They secrete antimicrobial peptides and thus control the colonization of the skin. At the same time, they have a repertoire of so-called "pattern recognition receptors" [23] and are thus active in an immunological sense [24].
The question that arises naturally: how must the skin be colonized in order to be healthy? The description of a healthy microbiome, however, is relatively difficult, since its compositions are so individual. Furthermore, no absolute data are published on the bacterial load of healthy skin and possible changes due to lifestyle or disease.
However, it is known that the more diverse the colonization and the quicker the system recovers after disturbances, the better / healthier it is [25].
Therefore, it is easier to assign certain organisms to certain skin diseases. For example, in Atopic Dermatitis it is known that Staphylococcus aureus is found in increasing numbers on the skin, especially in the diseased areas [16, 26].
Staphylococci also play a role in acne and rosacea, as they increasingly colonize the skin whenever the pH is shifted slightly upwards. In the case of acne and rosacea mites [27] and propionibacterium acnes (but only certain representatives) are also discussed as triggers of the disease [28-31].
Also the fungus Malassezia is also an organism found in all human beings. It is considered a so-called opportunistic germ, which sometimes becomes pathogenic. Then it is responsible for dandruff (scalp) or seborrheic dermatitis [32].
Pro- and prebiotic skincare, does it make sense?
Of course, we influence our skin microbiome with our daily hygiene and care habits [33], although unknowingly.
This is particularly clear and relatively well researched in the area of the armpit. There, the use of deodorants or antiperspirants reduces the number of corynebacteria that contribute most to odour formation [34-37].
Other applications include balneotherapy (38) and certain products for atopic dermatitis [39, 40].
Recently, more and more cosmetic products are launched that claim to have a positive effect on the skin microbiome. As a rule, they contain pro-and prebiotic substances, which we also know from food. Efforts to convince the FDA (the US regulatory body of medicine/cosmetics) of a claim regarding the microbiome are also evident in the USA. I am very sceptical as to whether this makes sense because so far no standard investigation methods for the microbial colonization of the skin are established and on the other hand the FDA could come up with the idea to classify this claim as medical [41]. That would not help anyone, at least in cosmetics.
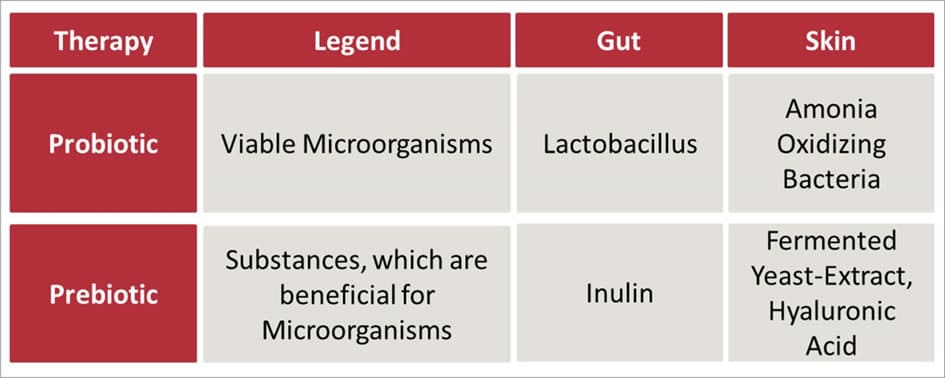
Table 2: Probiotic and prebiotic approaches to improve the microbiome. While these approaches to improve the gut microbiome are already established, they are comparatively new to the skin microbiome. In 2014 a real hype was created in the US by a publication in the New York Times, which published a review on the use of bacteria to restore the skin's microbiome [42].
But before we continue to lubricate our skin with further products, we should maybe leave some out. These include antibiotics that definitely damage the microbiome of the skin. The repeated use of bacteriostatic products for hand hygiene is unfavourable (occupational dermatoses). Also, frequent washing with irritating surfactants is unfavourable, as well as a long-term shift in skin pH or long-wearing of air-impermeable gloves. Depending on the individual's predisposition, this can lead to long-term shifts in the composition of the microbiome of the skin.
The gut-skin-axis: Why nutrition is so important
Recent research seems to confirm what was postulated many years ago. How we nourish ourselves not only affects the microbiome in the gut but also the appearance of our skin [43].
The gut microbiome has been comparatively well studied (Table 1). One can pin typical lifestyle diseases such as diabetes, obesity or irritable bowel syndrome to a change in the colonization of the gut. The findings were also confirmed for asthma and atopic dermatitis [44]. It is believed that the microorganisms located in the gut secrete or mobilize biochemical messengers that act on the immune system and can also activate signalling cascades in the skin. This so-called gut-skin axis is increasingly being discussed in acne and atopic dermatitis [45]. And it seems that there is something on it.
The so-called detoxification or fasting affects not only personal well-being but also the appearance of the skin. And so probiotic and prebiotic substances really make sense in nutrition.
Conclusion
With our skincare habits, we have always been influencing the skin microbiome for years without being aware of it. Now, the sudden use of products to improve the skin microbiome in an uncontrolled manner does not make sense from my point of view. I would rather reflect on which substances or habits are actually harmful and then let them be. If you want to do something good for the skin, then a diet that uses more fibre and reduces meat, dairy and alcohol can help. But that is not new...
References
(1) https://ghr.nlm.nih.gov/primer/hgp/accomplishments
(2) https://www.genome.gov/11006929/
(3) https://en.wikipedia.org/wiki/Human_Genome_Project#Findings
(4) https://www.theguardian.com/science/2010/oct/27/1000-genomes-project-genetic-variation
(5) The Lancet Infectious Diseases Commission, Antibiotic resistance—the need for global solutions. The Lancet, Infectious diseases, (2013) 13 (2): 1057-1098. http://www.sciencedirect.com/science/article/pii/S1473309913703189
(6) http://www.zeit.de/wissen/gesundheit/2017-05/multiresistente-keime-tuberkulose-antibiotika-medizin-forschung-tbc-resistenzen
(7) http://www.who.int/mediacentre/factsheets/fs104/en/
(8) https://en.wikipedia.org/wiki/Taxonomy_(general)
(9) Meisel, Jacquelyn S. et al., Skin Microbiome Surveys Are Strongly Influenced by Experimental Design, Journal of Investigative Dermatology, Volume 136 , Issue 5 , 947 – 956 (2016) https://www.med.upenn.edu/gricelab/assets/user-content/documents/Papers/2016/Skin%20Microbiome%20Surveys%20Are%20Strongly%20Influenced%20by%20Experimental%20Design.pdf
(10) Lloyd-Price J, Abu-Ali G, Huttenhower C. The healthy human microbiome, Genome Medicine (2016) 8:51. doi:10.1186/s13073-016-0307-y. https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-016-0307-y
(11) https://www.haut.de/glossar/barrierefunktion/?highlight=hautbarriere
(12) https://www.pinkmelon.de/magazin/geheimnis-kosmetik/helfen-ceramide-wirklich.html
(13) http://www.dejayu.de/den-uv-index-nutzen-hautkrebs-vermeiden/
(14) http://www.dejayu.de/kosmetische-hauttypen-mythos-chaos-und-neueste-erkenntnisse/
(15) https://www.med.upenn.edu/gricelab/
(16) Byrd LA, Belkaid Y, Segre JA, The human skin mircobiome, Nature Reviews Microbiology 16:3 (2018) 143-155. doi:10.1038/nrmicro.2017.157 https://www.nature.com/articles/nrmicro.2017.157 (17) Belkaid Y, Segre JA, Dialogue between skin microbiota and immunity, Science 346:6212, 954-959 (2014) https://science.sciencemag.org/content/346/6212/954
(18) Dominguez-Bello MG, Godoy-Vitorino F, Knight R, et al., Role of the microbiome in human development, Gut 2019;68:1108-1114. https://gut.bmj.com/content/68/6/1108
(19) Oh, J, Byrd, AL, Deming, C, Conlan, S, NISC Comparative Sequencing Program, Kong, HH, Segre, JA, Biogeography and individuality shape function in the human skin metagenome, Nature 514, 59-64 (2014) https://www.nature.com/articles/nature13786
(20) Dorrestein PC, Gallo RL, Knight R, Microbial Skin Inhabitants: Friends Forever, 165:4, 771-772 (2018) https://linkinghub.elsevier.com/retrieve/pii/S0092-8674(16)30478-0
(21) Gao Z, Perez-Perez GI, Chen Y, Blaser MJ. Quantitation of major human cutaneous bacterial and fungal populations. J Clin Microbiol. 2010;48(10):3575–3581 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2953113/
(22) Grice EA, Segre JA, The skin microbiome. Nat Rev Microbiol (2011) 9(4): 244-253.
doi: 10.1038/nrmicro2537. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3535073/
(23) https://www.rndsystems.com/resources/posters/pattern-recognition-receptors-innate-immune-response
(24) Sanford JA, Gallo RL. Functions of the skin microbiota in health and disease. Semin Immunol. 2013;25(5):370–377. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4219649/
(25) Findley K, Williams DR, Grice EA, Bonham VL, Health Disparities and the Microbiome, Trends in Microbiology, 24:11, 847-850 (2016) https://www.med.upenn.edu/gricelab/assets/user-content/documents/Papers/2016/Health%20Disparities%20and%20the%20Microbiome.pdf
(26) Findley K, Grice EA, The Skin Microbiome: A Focus on Pathogens and TheirAssociation with Skin Disease, PLOS Pathogens, 10:11. 1004436 (2014) https://www.med.upenn.edu/gricelab/assets/user-content/documents/Papers/2014/Skin%20microbiome-%20a%20focus%20on%20pathogens%20and%20their%20association%20with%20skin%20disease.pdf
(27) Sarangua TS, Gurbadam A, Enkhtur YA, Correlation Demodex Folliculorum and Skin Biophysical Parameters, Journal of Cosmetics, Dermatological Sciences and Applications, 3:3 (2013), https://file.scirp.org/pdf/JCDSA_2013092511513193.pdf
(28) Tomida S, Nguyen L, Chiu B, Liu J, Sodergren E, Weinstock GM, Li H. Pan-genome and comparative genome analyses of Propionibacterium acnes reveal its genomic diversity in the healthy and diseased human skin microbiome. mBio (2013) 4(3):e00003-13.
doi:10.1128/mBio.00003-13. https://mbio.asm.org/content/4/3/e00003-13.short
(29) Fitz-Gibbon S, Tomida S, Chiu BH, Nguyen L, Du C, Liu M, Elashoff D, Erfe MC, Loncaric A, Kim J, Modlin RL, Miller JF, Sodergren E, Craft N, Weinstock GM, Li H, Propionibacterium acnes Strain Populations in the Human Skin Microbiome Associated with Acne, Journal of Investigative Dermatology (2013), 133 (9): 2152-2160.
https://doi.org/10.1038/jid.2013.21.
(30) Tanghetti EA. The role of inflammation in the pathology of acne. J Clin Aesthet Dermatol.6:9, (2013), 27-35. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3780801/
(31) Lheure C, Grange PA, Ollagnier G, Morand P, Désiré N, Sayon S, et al., TLR-2 Recognizes Propionibacterium acnes CAMP Factor1 from Highly Inflammatory Strains, PLoSONE 11(11):e0167237 (2016) .doi:10.1371/journal.pone.0167237 https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0167237
(32) Kim GK. Seborrheic Dermatitis and Malassezia species: How Are They Related?. J Clin Aesthet Dermatol. 2009;2(11):14–17. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2923939/
(33) Rosenthal M, Goldberg D, Aiello A, Larson E, Foxman B. Skin microbiota: microbial community structure and its potential association with health and disease. Infect Genet Evol. 2011;11(5):839–848. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3114449/
(34) https://www.pinkmelon.de/magazin/geheimnis-kosmetik/schweissgeruch-und-wie-deos-wirken.html
(35) Callewaert C, Kerckhof F-M, Granitsiotis MS, Van Gele M, Van de Wiele T, Boon N (2013) Characterization of Staphylococcus and Corynebacterium Clusters in the Human Axillary Region. PLoS ONE 8(8): e70538. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0070538
(36) Callewaert C , Hutapea P, Van de Wiele T, Boon N, Deodorants and antiperspirants affect the axillary bacterial community, Archives of Dermatological Research 306:8, 701-710 (2014) https://link.springer.com/article/10.1007/s00403-014-1487-1
(37) Urban J, Fergus DJ, Savage AM, Ehlers M, Menninger HL, Dunn RR, Horvath JE, The effect of habitual and experimental antiperspirant and deodorant product use on the armpit microbiome, PeerJ 4:e1605 (2016) http://macroecointern.dk/pdf-reprints/Urban_PeerJ_2016.pdf
(38) http://www.dejayu.de/mit-dreck-heilen-was-mit-schlamm-so-alles-geht/
(39) Bjerre, R, Bandier, J, Skov, L, Engstrand, L, Johansen, J, The role of the skin microbiome in atopic dermatitis: a systematic review. Br J Dermatol (2017), 177: 1272-1278 https://onlinelibrary.wiley.com/doi/pdf/10.1111/bjd.15390
(40) Flores, GE, Seité, S, Henley JB, et al., Microbiome of Affected and Unaffected Skin of Patients With Atopic Dermatitis Before and After Emollient Treatment, Journal of Drugs in Dermatology 13:11, 611-618 (2014) https://skinmiles.com/wp-content/uploads/2017/12/La-Roche-Posay-Lipikar-and-Microbiome.pdf
(41) http://www.dejayu.de/strivectin-sd-konzentrat-kosmetisch-oder-pharmakologisch-gegen-falten-wirksam/
(42) https://www.nytimes.com/2014/05/25/magazine/my-no-soap-no-shampoo-bacteria-rich-hygiene-experiment.html?mcubz=3
(43) Salem I, Ramser A, Isham N, Ghannoum MA. The Gut Microbiome as a Major Regulator of the Gut-Skin Axis. Front Microbiol. 2018;9:1459. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6048199/
(44) Iemoli E, et al, Probiotics Reduce Gut Microbial Translocation and Improve Adult Atopic Dermatitis, J Clin Gastroenterol 2012;46:S33–S40 https://pdfs.semanticscholar.org/271e/c6dbab1209cb3908af07bd474dffefa15ec5.pdf
(45) Lee SY, Lee E, Park YM, Hong SJ. Microbiome in the Gut-Skin Axis in Atopic Dermatitis. Allergy Asthma Immunol Res. 2018 Jul;10(4):354-362 https://synapse.koreamed.org/search.php?where=aview&id=10.4168/aair.2018.10.4.354&code=0166AAIR&vmode=FULL
Additional links
Human Microbiome Project: https://hmpdacc.org/.
Figure 1: Logo of the Human Microbiome Project https://hmpdacc.org/
All other figures and tables are own works and can be used under the Cerative Commons Licence CC BY-SA 3.0