By Elena HERNANDEZ
Ph.D. (Russia–Israel) Biologist, biophysist
Editor-in-chief of the Cosmetics & Medicine Publiching (Russia)
Chair of the Board of International Association for Applied Corneotherapy (I.A.C.)
Three stars of corneotherapy - barrier lipids, antioxidants, hyaluronic acid - all important in maintaining homeostasis of the epidermis.
Corneotherapy is a part of modern cosmetology and dermatology, in which special attention is paid to the condition of the stratum corneum and maintaining its barrier function.
This article presents a complex therapy program that includes strengthening the lipid barrier of the stratum corneum by applying a mixture of barrier lipids, normalizing the immune status of the skin with topical antioxidants, and restoring the water balance of the epidermis with hyaluronic acid.
GOOD BARRIER= HEALTHY SKIN= BEAUTIFUL SKIN
The stratum corneum is primarily a mechanical shield that reflects external shocks. But its protective function is not limited to this [1]. The stratum corneum also controls the passage of chemicals in both directions -from outside to inside and from inside to outside. Substances such as oxygen and carbon dioxide do this unhindered along a concentration gradient from an area where there is more of a given substance to where it is less. Water passes through the stratum corneum towards the surface, also along a concentration gradient. However, its movement is controlled by special structures within the stratum corneum - the lipid barrier and natural moisturizing factor, as well as the hydrolipid mantle.
The permeability of the skin to oxygen, carbon dioxide and water is of great physiological importance. As for other substances, the passage is "closed" for them a normal stratum corneum with the correct barrier structures will not let anything pass through itself just like that. Small (molecular weight up to 500 Da) fat-soluble molecules (for example, phospholipids, retinol), which are similar in size and physiochemical properties to barrier lipids, have a high chance to pass through the barrier. Water-soluble substances, even small ones, simply cannot pass through an intact barrier; for this, special measures must be taken to change the structure of the barrier.
What is the danger of physical damage or chemical changes in the barrier structures of the stratum corneum? The fact that living skin cells remain without outer shield.
From the external environment, foreign agents can get to them chemical (pollutants, house dust, cosmetic components, etc.) or biological (microorganisms).
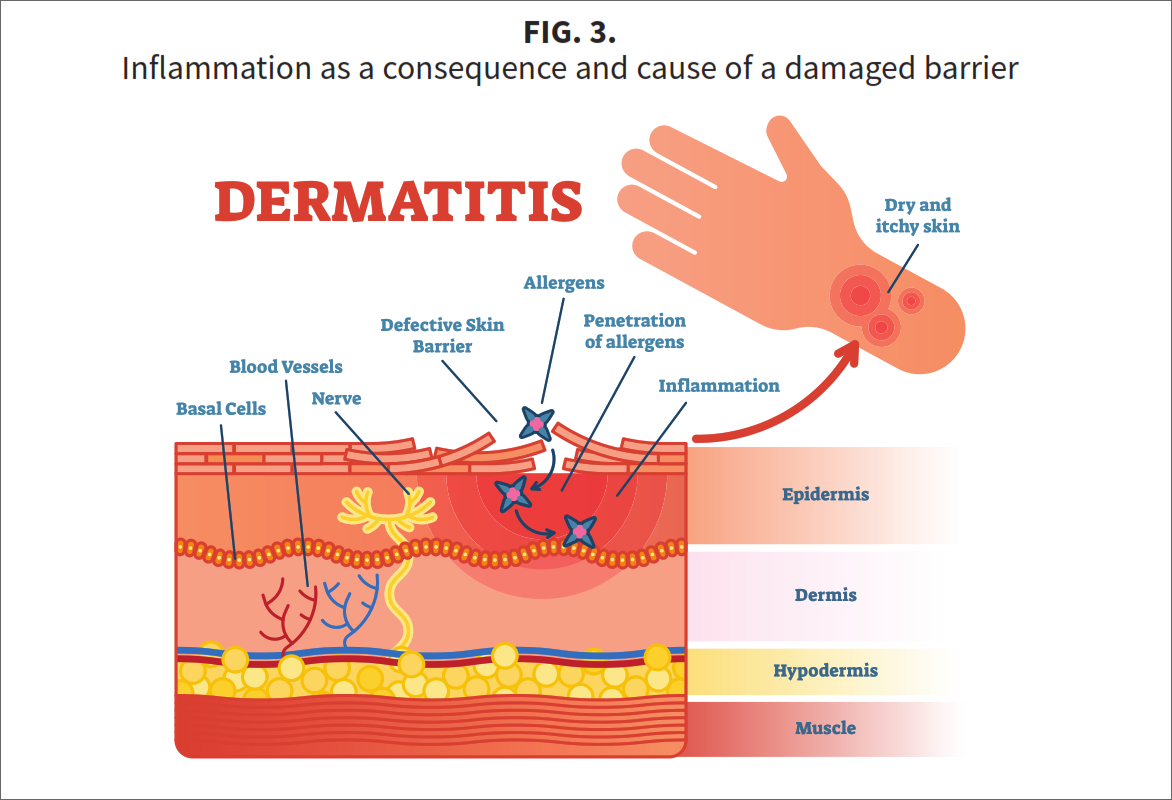
To remove pathogens from the living layers of the skin, the immune system of the skin is involved, and then inflammation develops with characteristic signs: redness, swelling, pain and even itching are possible.
Acute inflammation is the normal response of the skin to injury. It performs at least two important tasks: firstly, it protects against pathogens that enter the skin through a damaged or weakened barrier, and secondly, it triggers wound healing, a complex multi-stage process during which the integrity of the skin is restored. As the skin in general and its barrier in particular heal, the inflammation subsides (Fig. 1). This is normal. But there are situations when the inflammatory process cannot resolve itself.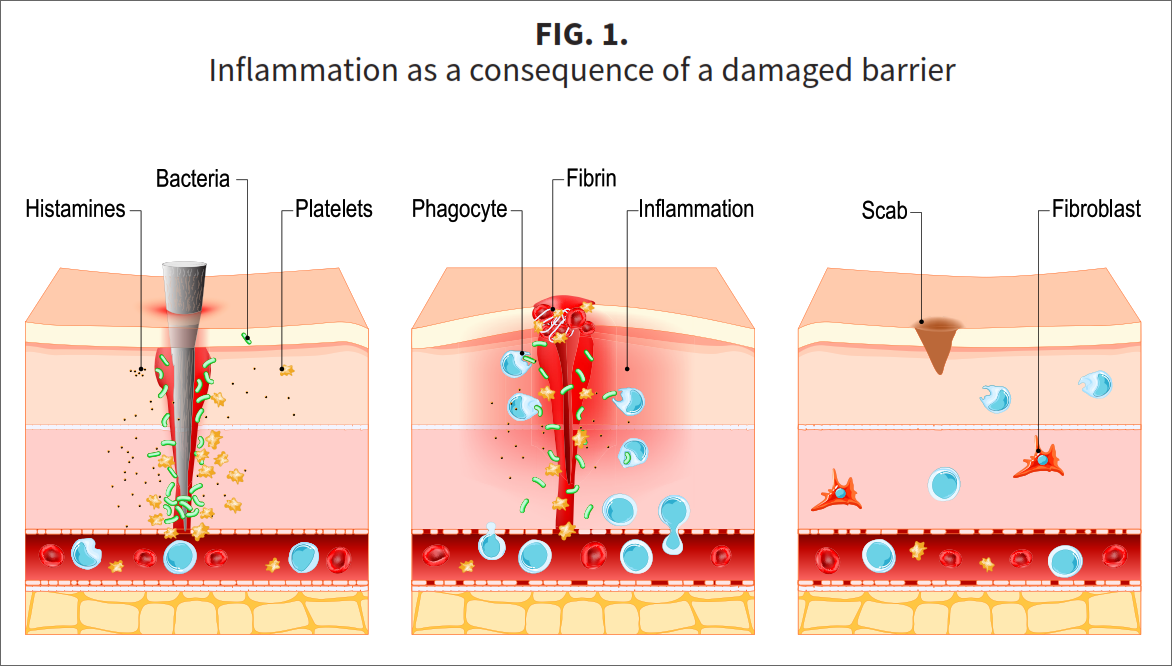
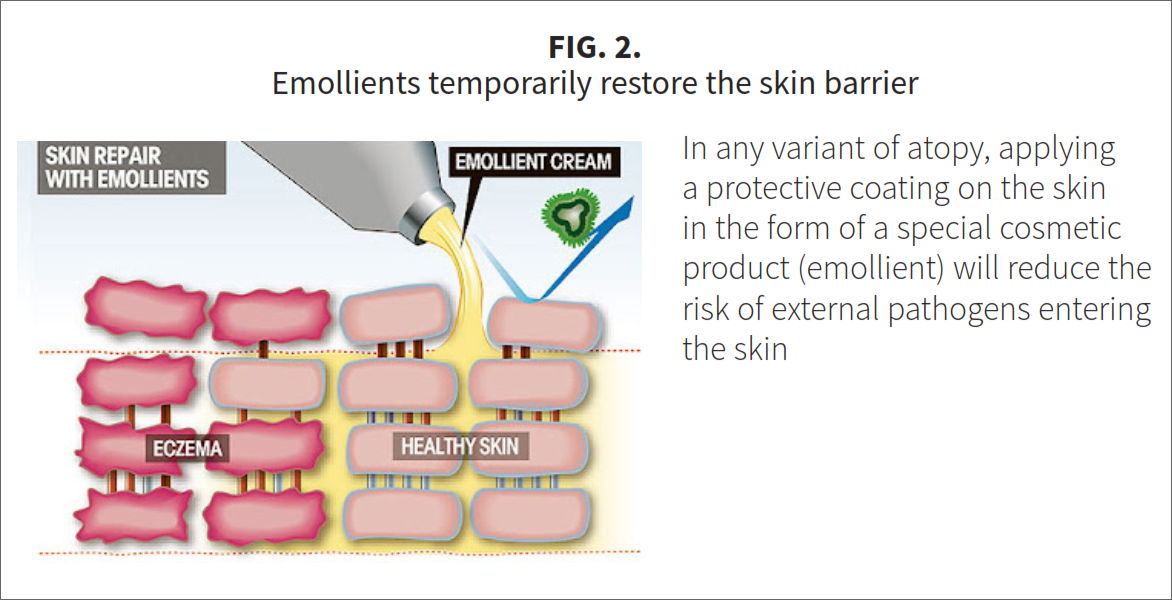
For example, in case of atopic dermatitis, the keratinization process is disrupted at the genetic level; these patients are born and live all their lives with an incorrectly formed weak barrier [2]. Therefore, their skin reacts to a wide variety of external influences with an outbreak of inflammation. To date, about 30 mutations have been identified that lead to the clinic of atopic dermatitis. The frequency of outbreaks and the severity of the course depends on which mutation a particular patient has. In more severe cases, in addition to the "wrong" barrier, there are significant changes in the functioning of the immune system, and then it is more difficult to extinguish outbreaks of inflammation. But in any variant of atopy, applying a protective coating to the skin in the form of a special cosmetic product, which essentially acts as a barrier, will reduce the likelihood of external pathogens entering the skin. Dermatologists call such special products emollients (Fig. 2).
Another example is allergic contact dermatitis. This dermatosis is provoked by a pathogen to which the immune system reacts too violently. Inflammation can be so severe that itching often occurs on the affected area, the person actively itches and additionally injures the stratum corneum. Through damage to the barrier, other pathogens begin to enter and maintain inflammation. Thus, acute inflammation becomes chronic (Fig. 3).
Microcirculation and drainage are disturbed in the zone of chronic inflammation (Fig. 4). As a result, living cells find themselves in conditions of stagnation - they receive less nutrients and oxygen, and the products of cellular metabolism become heated in the intercellular medium and slagging it. The life of all skin cells in the focus of chronic inflammation is inhibited, including the life of keratinocytes.
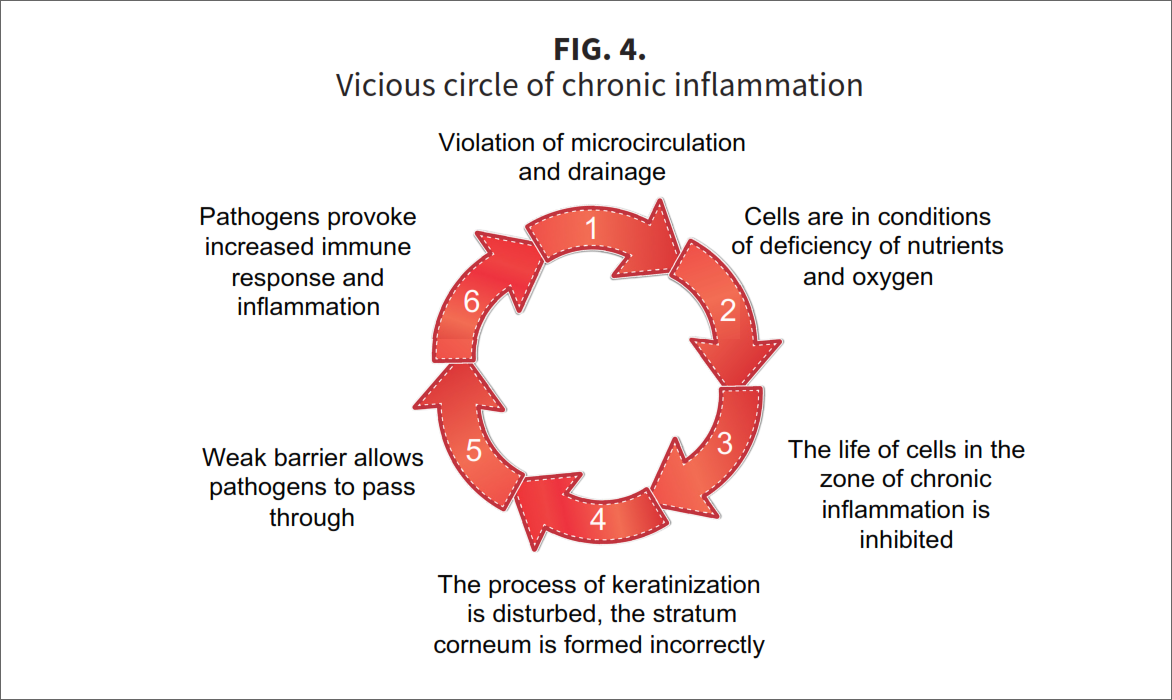
Under these conditions, they cannot develop normally and form the correct stratum corneum. Therefore, over the area of chronic inflammation, the barrier is weak and passes through itself what a healthy stratum corneum will not let through. Other pathogens begin to enter the skin, to which the immune response is triggered, and this further exacerbates inflammation. It turns out a vicious circle, where it is already difficult to say what is primary and what is secondary.
Obvious clinical examples of such closed states can serve as chronic inflammatory dermatoses such as acne, seborrheic dermatitis, rosacea. The causes of these diseases are different, but they are related by chronic inflammation and a weak barrier. Therefore, outwardly, they may be similar (especially acne and rosacea in papulo-pustular form are often confused).
How to prevent the emergence of a vicious circle or how to interrupt it, if it nevertheless appeared? The answer is obvious -you need a reliable stratum corneum with the right barrier. With all skin pathologies and conditions "deviation from the norm", the barrier suffers in one way or another. Therefore, when working with the skin, you should always remember the stratum corneum -this is the universality of the corneotherapeutic approach.
Corneotherapy sets a good barrier as its main goal.
• If the barrier is damaged, it must be repaired.
• If it is weakened, then strengthen it.
• If there is a possibility that external impacts are too strong and the barrier will not withstand them, then it must be additionally protected.
The most effective way to work with the stratum corneum is with the help of cosmetic products that are applied to the surface of the skin and come into direct contact with the stratum corneum and the hydrolipid mantle. That is why cosmetics is the main tool of corneotherapy.
KEY INGREDIENTS OF CORNEOTHERAPY COSMETICS
Substances applied to the skin as part of cosmetics remain on its surface, mixing with the hydrolipid mantle. The smallest can penetrate into the stratum corneum to its different depths, where they accumulate, and when the time comes, they leave the surface of the skin together with the horny scales. If the barrier structures of the stratum corneum are altered and/or if its integrity is compromised as a result of injury, then some cosmetic ingredients may pass through the stratum corneum and reach living cells.
What substances do skin with a damaged or weakened barrier need and why? Let's figure it out.
Barrier lipids
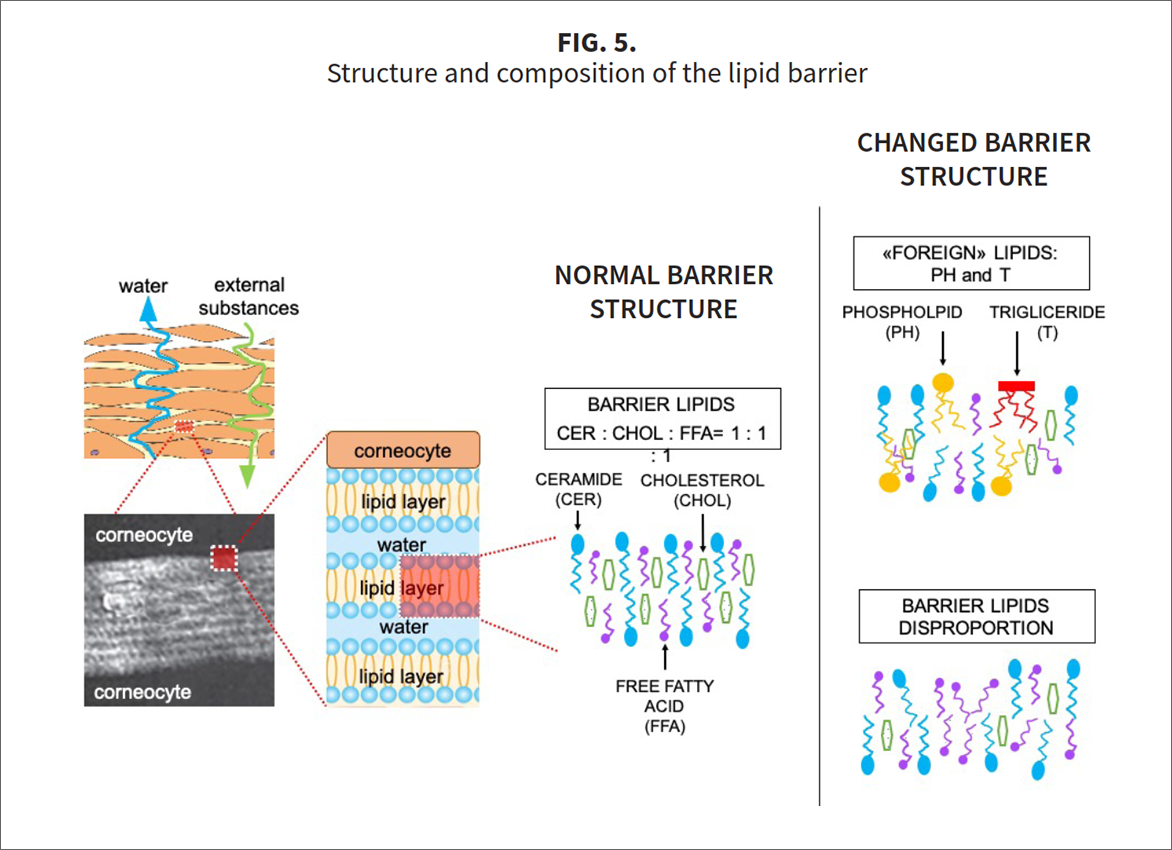
The main route of diffusion of substances through the stratum corneum lies between the stratum corneum. This space is filled with a structure known as the lipid barrier. The lipid barrier consists of lipid layers parallel to each other, separated by a thin layer of water.
Normally, the layers are composed of three groups of lipids, taken in almost the same proportion: ceramides (CER), cholesterol (CHOL), free fatty acids (FFA) [3]. If this proportion changes, then the entire structure of the barrier also changes -pores and even gaps appear in it, it ceases to restrain the evaporation of water, and the stratum corneum begins to lose moisture (Fig. 5). The clinical symptoms of dryness of the stratum corneum are a feeling of tightness, visible peeling, increased irritability [4].
The most common causes of changes in the proportion of barrier lipids:
1) skin aging [5, 6];
2) regular and frequent washing of the skin using traditional soap having a pH>9 (suppression of the activity of stratum corneum enzymes involved in the collection of the lipid barrier);
3) frequent rubbing of the skin with an ethanol solution ("washing out" of lipids from the intercellular spaces of the stratum corneum);
4) regular use for a long time of undiluted vegetable oil (any), enriched with triglycerides and phospholipids (replacement of barrier lipids with lipids that are not normally present in the barrier);
5) vegetarianism and fat-reducing diets (nutritional deficiency of certain lipids, such as unsaturated fatty acids and ceramides);
6) congenital disorder (atopic dermatitis);
7) some hormonal diseases and conditions, for example, diabetes, hypothyroidism, menopause (impaired lipid metabolism in the skin).
Antioxidants
If problems with the barrier have been observed for a long time, such skin is almost certainly hypersensitive. It is characterized by signs of inflammation, such as redness, burning sensation, and sometimes itching.
In the site of inflammation, the level of oxidizing agents (reactive oxygen species and free radicals) rises sharply, and the own antioxidant system can no longer cope with its main task to maintain a balance between oxidizing agents and reducing agents. This condition is called oxidative stress, and it accompanies and maintains inflammation.
Reinforcement of the skin's own antioxidant system in the form of topical antioxidants will help to bring the situation under control inflammation decreases, the skin calms down and can normally take up construction work, including at the barrier level [7]. Therefore, corrective lipid therapy should be combined with topical antioxidants in situations where inflammation is already present or when a damaging cosmetic procedure is expected, after which inflammation will definitely occur [8].
Indications for topical antioxidants:
1) for the prevention and correction of age-related skin changes associated with oxidative stress (pigmentation, reduced elasticity and superficial vascular network as a result of glycation of structural proteins collagen and elastin).
2) acute inflammatory reaction (photodamage, injury);
3) before and after damaging cosmetic procedures;
4) chronic dermatoses of different etiology and pathogenesis (atopic dermatitis, psoriasis, acne, seborrheic dermatitis, rosacea).
Hyaluronic acid
Another constant companion of the "weak barrier" problem is the lack of water in the stratum corneum, and in advanced cases, in the epidermis itself. In the area under the weakened stratum corneum, the living cells of the epidermis are in conditions of water deficiency. Signs of a violation of the water balance of the epidermis are poor healing and delayed epithelialization, as well as keratosis, texture roughness, superficial wrinkles, and visible peeling.
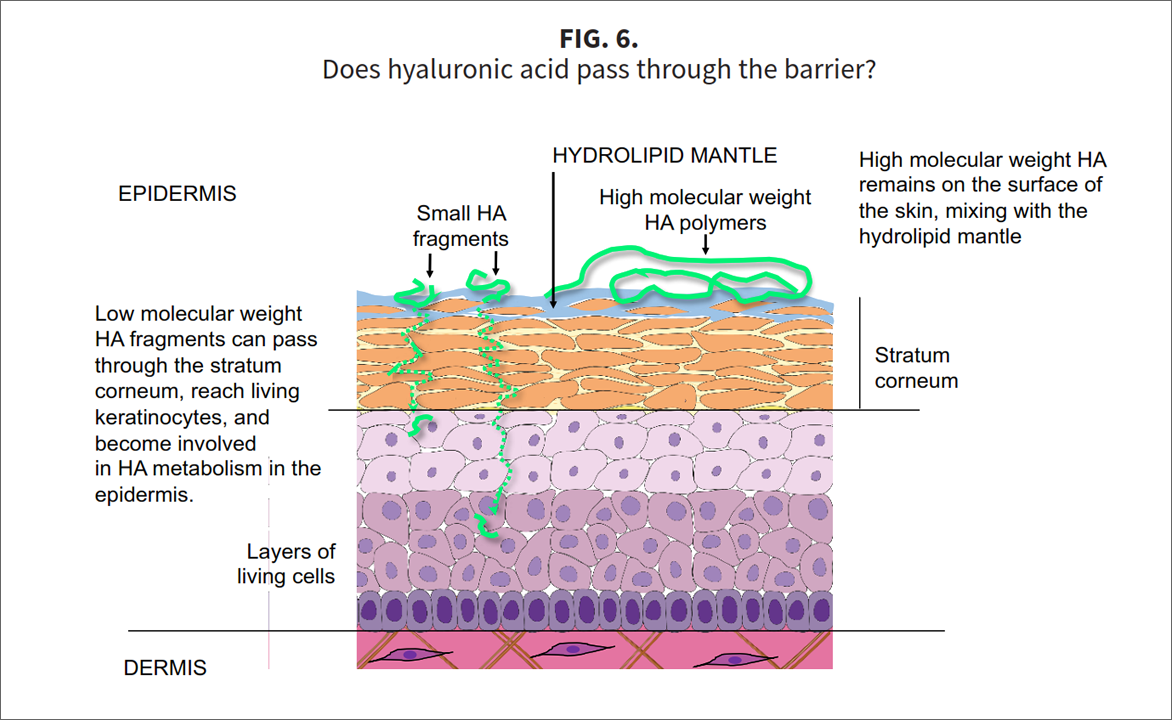
To restore the water balance both at the level of the stratum corneum and the living layers of the epidermis, topical formulations with native hyaluronic acid (HA) of different molecular weights can be used [9]. After application to the skin, high molecular weight HA (> 1 million Da) remains on the surface, mixing with the hydrolipid mantle and moisturizing the stratum corneum according to the "wet compress" principle. Low molecular weight HA can pass through the barrier if it is physically damaged [10]. Under the stratum corneum, small fragments of HA are captured by keratinocytes. They use these fragments as a building material for the synthesis of their own high-molecular-weight HA, which fills the intercellular spaces of the epidermis and participates in the regulation of water balance in it. The hyaluronic sheath around keratinocytes thickens as cells migrate during epithelialization and wound healing (Fig. 6).
In the case of dry xerotic cracked skin with a damaged barrier, ready to flare up on any external impact, topical HA will be of real help: high molecular weight HA will create a moist coating on the surface, soften the skin, relieve the feeling of tightness. And low molecular weight HA will maintain the water balance of the living layers of the epidermis and improve healing.
Indications for the use of topical HA:
1) age-related and constitutional dry skin;
2) xerosis;
3) hypersensitivity;
4) delayed epithelialization;
5) to improve recovery after damaging cosmetic procedures.
PRACTICAL RECOMMENDATIONS
The effectiveness of corneotherapy depends not only on the selected drugs. It is important to apply them correctly.
Below are 4 general recommendations.
Rule# 1. Application sequence
Most of the antioxidants used in cosmetics are water soluble. Therefore, products with a fairly high concentration of antioxidants are often aqueous solutions or gels, less often liposomal suspensions. To emphasize their relatively high concentration of antioxidants, such products may be referred to as Serums or Concentrates on the market. In any case, there is a lot of water in them. After application to the skin, the water evaporates quickly, and a feeling of tightness may appear.
The same applies to hyaluronic acid, which does not dissolve in fat, but swells in water, forming a gel. After the water evaporates, its polymer chains dry up and begin to cling to the skin. The result is an unpleasant feeling of tightness. To avoid it, first apply a serum (antioxidant or hyaluronic), then a cream with lipids.
Rule# 2. Serum selection
Hyaluronic acid (HA) is best applied in the morning, since high molecular weight HA creates an additional protective coating, during the day it is more relevant. If the skin is damaged, then both forms of HA should be present in the preparation (high and low molecular weight). If there is no damage, just symptoms of dryness, then only high molecular weight HA is sufficient.
In the evening, the skin should be soothed, so the choice here will be in the direction of topical antioxidants. There are a big variety of antioxidant concentrates in the market, differing in the antioxidant composition and base form. So, there is a possibility to choose topical antioxidant product taking into account the activity of sebum secretion and such clinical signs as a tendency to pigmentation and the severity of inflammation.
Rule# 3. Skin preparation and application method
First of all, the skin must be cleansed with a special cleanser, selected according to the type of sebum secretion and balanced in pH.
The cleanser must be applied to moistened skin and spread over its surface with soft circular movements. Then the skin must be thoroughly rinsed with warm water and lightly blotted with a soft towel. It is impossible to rub or dry the skin, because we are dealing with a weakened barrier, and it does not need additional mechanical trauma.
Apply serum to wet skin and, lightly tapping with fingertips, distribute it evenly over the entire face. Let the serum absorb a little, but do not dry out - the skin should not be sticky or dry. Then we apply a cream with lipids on slightly moistened skin, spread it easily without rubbing.
Rule #4. UV Protection
10-15 minutes after morning application of the cream, if necessary, you can apply foundation or sunscreen with mineral UV filters, selected according to skin type.
SUMMARY
Since the goal of corneotherapy is to maintain the protective function of the skin, it can be successfully used to solve various aesthetic and dermatological problems:
1) non-invasive treatments that restore the three lines of skin barrier defence that do not ablate (remove) the epidermis
1) prevention of aging as a monotherapy;
2) correction of age-related skin changes -together with intensive cosmetological treatments (Phototherapy (LED), Collagen induction therapy (CIT), Iontophoresis & Sonophoresis, Microcurrent, Enzymes, Intense pulsed light (IPL), Long pulsed laser);
3) prevention of pathology as monotherapy or as a part of in a preventive medical treatment;
4) treatment of skin diseases and conditions together with drug therapy;
5) treatment of skin diseases and conditions – together with drug therapy or adjuvant medical treatment.
The key component of the corneotherapy program are barrier lipids -ceramides, cholesterol, polyunsaturated fatty acids. If necessary, they should be combined with topical
antioxidants and hyaluronic acid (high and low molecular weight), which will more effectively soothe the skin and restore its water balance.
Whatever the reason for the weakness of the barrier, the skin will thank you for this help!
REFERENCES
1. Madison K.C. Barrier function of the skin: "la raison d'~tre" of the epidermis. J Invest Dermatol. 2003; 121(2):231-241.
2. van Smeden J., Bouwstra J.A. Stratum Corneum Lipids: Their Role for the Skin Barrier Function in Healthy Subjects and Atopic Dermatitis Patients. Curr Probl Dermatol. 2016; 49: 8-26.
3. van Smeden J., Janssens M., Gooris G.S., Bouwstra J.A. The important role of stratum corneu m lipids for the cutaneous barrier function. Biochim Biophys Acta. 2014; 1841(3): 295-313.
4. Proksch E., Berardesca E., Misery L., et al. Dry skin management: practical approach in light of latest research on skin structure and function. J Dermatolog Treat. 2020; 31(7): 716-722.
5. Elias P.M. Ghadially R. The aged epidermal permeability barrier: basis for functional abnormalities. Clin Geriat Med. 2002; 18(1): 103-120.
6. Wang Z., Man M.Q., Li T., et al. Aging-associated alterations in epidermal function and their clinical significance. Aging (Albany NY). 2020; 12(6): 5551-5565.
7. Thiele J.J., Schroeter C., Hsieh S.N., et al. The antioxidant network of the stratum corneum. Curr ProblDermatol. 2001; 29: 26-42.
8. Thiele J.J. Oxidative targets in the stratum corneum. A new basis for antioxidative strategies. Skin Pharmacol Appl Skin Physiol. 2001;14(Suppl 1): 87-91.
9. Zhu J, Tang X, Jia Y, et al. Applications and delivery mechanisms of hyaluronic acid used for topical/transdermal delivery --A review. Int J Pharm. 2020; 578: 119127.
10. Essendoubi M., Gobi net C., Reynaud R., et al. Human skin penetration of hyaluronic acid of different molecular weights as probed by Raman spectroscopy. Skin Res Technol. 2016, 22(1): 55-62.